G???s duvar?nda miksofibrosarkomal? bir olgu
Hatice
Canan HASANO?LU1, Ay?eg?l KARALEZL?1, Elif TANRIVERD?O1,
Mehmet G?M??2,
Mehtap AYDIN3
1 SB Ankara Atat?rk E?itim ve Ara?t?rma Hastanesi, G???s Hastal?klar? Klini?i, Ankara,
2 SB Ankara Atat?rk E?itim ve Ara?t?rma Hastanesi, Radyoloji Klini?i, Ankara,
3 SB Atat?rk G???s Hastal?klar? ve G???s Cerrahisi E?itim ve Ara?t?rma Hastanesi, Patoloji Klini?i, Ankara.
?ZET
G???s duvar?nda miksofibrosarkomal? bir olgu
Fibrosarkoma malign fibroblastlar i?eren mezen?imal bir t?m?rd?r. Miksofibrosarkoma fibrosarkomun de?i?ken miksoid stroma, pleomorfizm ve geni? k?vr?ml? damarsal patern g?steren bir varyant?d?r. Hastal?k 6-8. dekadda s?kt?r, nadiren 20 ya? alt?nda g?r?l?r. ?o?u hasta yava? b?y?yen a?r?s?z kitle ile ba?vurur. Olgular?n ?o?unda t?m?r dermal/subk?tan dokudan geli?ir. ?nfiltratif veya s?n?rl? seyreder. T?m?r?n en s?k yerle?im yeri ekstremitelerdir (?zellikle alt ekstremiteler). Nadiren g?vde, kafa i?i ve boyun b?lgesinde yerle?ir. ?ngilizce literat?rde g???s duvar?nda miksofibrosarkomal? olguya rastlanmam??t?r. Biz bu bildiride g???s duvar?nda miksofibrosarkoma geli?en bir olgu sunduk.
Anahtar Kelimeler: Fibrosarkoma, miksofibrosarkoma, pulmoner malignite.
SUMMARY
A mass of myxofibrosarcoma in the lung
Hatice
Canan HASANO?LU1, Ay?eg?l KARALEZL?1, Elif TANRIVERD?O1,
Mehmet G?M??2,
Mehtap AYDIN3
1 Clinic of Chest Diseases, Ankara Ataturk Training and Research Hospital, Ankara, Turkey,
2 Clinic of Radiology, Ankara Ataturk Training and Research Hospital, Ankara, Turkey,
3 Clinic of Pathology, Ataturk Chest Diseases and Chest Surgery Training and Research Hospital,
Ankara, Turkey.
Fibrosarcoma is a mesenchymal tumor constituted by malignant fibroblasts. Myxofibrosarcoma is one of the fibrosarcoma variants that mostly develops from dermal/subcutaneous tissues. The most common locations are the limbs, with rare occurrences in the chest, head, and neck. Since, to best of our knowledge, there is no such report in English literature, we hereby present a case of lung myxofibrosarcoma. A 47-year-old man who had chest pain for 4 months was admitted to our clinic. The chest X-ray revealed a homogeneous density in the left upper lung. His chest computed tomography (CT) scan showed a solid mass lesion of 52 x 58 mm in size at the apical segment of the left upper lobe. There was tumor invasion at the second and third ribs. CT-guided fine-needle tru-cut lung biopsy was performed. Histopathological evaluation result was high grade myxofibrosarcoma. Surgery was conducted. Myxofibrosarcoma is a surgically curable disease. However, local recurrences occur in 50% to 60% of the cases. Therefore, chemotherapy and/or radiotherapy is the suggested approach following surgery.
Key Words: Fibrosarcoma, myxfibrosarcoma, pulmonary malignancy.
Fibrosarcoma is a mesenchymal tumor composed of malignant fibroblasts. Myxofibrosarcoma is one of the fibrosarcoma variants, and characterized by variable myxoid stroma, pleomorphism, and large curvilinear vascular pattern. This disease is frequent in patients on their 6th-8th decade, being rare under the age 20. Most of the patients admit to hospital with a slow developing, painless mass (1). In most of the cases, tumors are originated from dermal/subcutaneous tissues. Myxofibrosarcomas can be circumscribed or have an infiltrative growth pattern (1). Generally, these tumors are located in the limbs (especially lower limbs), and rarely on the chest, head, and neck (2).
To best of our knowledge, since there are no reports of myxofibrosarcomas located in the lung, this case was presented.
CASE REPORT
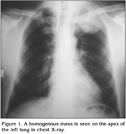
A 47-year-old male patient with chest pain complaints for 4 months and presenting effort dyspnea was admitted to our clinic. There was no pulmonary disease or tuberculosis in his clinical background. Although for 25 years he smoked 1 package of cigarettes a day, this habit had completely ceased 4 months before. In physical examination, the left hemithorax was more convex than the right hemithorax. There was no chest mass. There was an inspiratory rale on the right chest wall. Other examinations were normal. In laboratory analysis the results were white blood cell count (WBC) 11.400 KU/L, erythrocyte sedimentation rate (ESR) 39 mm/hour, antistreptolysin O (ASO) 260 IU/mL, C-reactive protein (CRP) 27.4 mg/L, serum calcium (Ca) 10.6 mg/dL, alanine aminotransferase (ALT) 87 mg/dL, aspartate aminotransferase (AST) 53 mg/dL, gamma glutamyltransferase (GGT) 88 U/L, lactate dehydrogenase (LDH) 596 U/L, creatin phosphokinase (CPK) 1086 U/L, creatine kinase MB (CK-MB) 37 U/L, and alkaline phosphatase (ALP) 382 U/L. Alpha-fetoprotein (AFP), cancer antigen (CA)-125, CA-15-3, CA-19-9, and carcinoembryonic antigen (CEA) results were normal. Evaluation through electrocardiography (ECG) evidenced Wolf Parkinson White syndrome. Chest X-ray revealed an increase of homogeneous density at the left upper lung lobe (Figure 1).
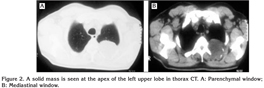
Thorax computed tomography (CT) revealed that the trachea, both of the main bronchus, the mediastinal main vascular structures, and the heart contour and size were normal. There was no pathologically developed lymph node on the mediastinum. Thorax CT scan indicated a solid mass lesion of 52 x 58 mm in size at the apical segment of the left upper lobe (Figure 2). Other lung parenchymal areas were normal. Cervical disc CT was applied in order to assess costal and vertebral invasion. T1, T2, T3 vertebra corpuses were evaluated as normal.
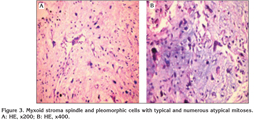
Tru-Cut lung biopsy was performed with CT from the mass. Histopathological evaluation revealed that the tumor was malignant mesenchymal: myxofibrosarcoma (Figure 3).
There was no metastatic lesion detected in abdominal ultrasonography (US), cranial magnetic resonance imaging (MRI), or bone scintigraphy of the patient. Surgery was performed. The neoplasm was composed of cellular fascicles of spindle and pleomorphic tumor cells with numerous, often atypical mitosis, and chest wall areas of hemorrhage and necrosis (Figure 3). Moreover, bizarre, multinucleated giant cells with abundant eosinophilic cytoplasm and irregular shaped nuclei was noted. There were necroses on five or six focal points. There were numerous convex vascular structures within the stroma. Immunohistochemical studies of stained tumor cells revealed diffuse positivity for vimentin and focal positivity for actin; desmin S100 and C68 stainings were negative. In histopathological evaluation, no tumor tissue was observed on the paravertebral muscle and costal ribs excised with the mass.
Ifosfamide and adriablastine chemotherapy was planned. The patient was treated by chemotherapy and radiotherapy with totally 60 Gray/30 fractions. After one year, thorax CT evaluation was normal.
DISCUSSION
Malignant fibrous histiocytoma (MFH) is a common subtype of soft tissue sarcomas, and myxofibrosarcoma was described as a distinct variant of MFH by Angervall et al. (3). Myxofibrosarcoma is one of the most common sarcomas in patients between their 6th and 8th decade, with a slight male predominance, as in our case (1,4).
The most common presentation of myxofibrosarcoma is a slowly enlarging, painless, subcutaneous swelling (1,5). The majority of these tumors arise from the limbs, especially the lower extremities. They are rarely seen on the chest (2,4). A previous report of chest myxofibrosarcoma described cutaneous presentation and dermal involvement (6). Our case consisted of a tumor located in the chest, but growing into the lung, which, as far as we acknowledge, has never been described.
The histological and immunohistochemical features of myxofibrosarcomas are characteristic. Histologic features include: commonly nodular growth pattern; a myxoid matrix containing elongated, curvilinear capillaries; and fusiform, round or stellate tumor cells with indistinct cell margins, slightly eosinophilic cytoplasm, and hyperchromatic atypical nuclei (3,4). Immunohistochemically, there is focal actin positivity in a minority of cases. With exception to consistent vimentin staining, all other routinely used markers are negative (1). Histological and immunohistochemical examinations of our case were characteristic of myxofibrosarcoma.
These tumors have been subdivided into four grades based on the degree of cellularity, the nuclear pleomorphism, areas of necrosis, and the mitotic activity (4). Our case was established as "grade II myxofibrosarcoma" according to these criteria.
Local recurrences occur in up to 50-60% of the cases independently of histological grading (1). Intermediate -and high- grade neoplasms may develop hematogenous metastases in about 20-35% of the cases (4,7). Additionally, a significant proportion of myxofibrosarcomas that deceivingly appear circumscribed in growth actually present microscopic extension of individual sarcoma cells along the fasicoaponeurotic plane. Tumor progression with increased metastases is frequently seen after relentless local recurrences, especially when resection margins are positive in primary surgery (8). Therefore, chemotherapy and/or radiotherapy is the recommended approach following surgery (5,7). We planned chemotherapy and radiotherapy in our case.
As conclusion, in myxofibrosarcoma, early diagnosis and surgical treatment are significant for prognosis. Although the tumor can be curable by surgery, local recurrences may occur in 50-60% of the cases. For this reason, chemotherapy and/or radiotherapy can be prescribed to the patients after the surgical procedure.
CONFLICT of INTEREST
None declared.
REFERENCES
- Mentzel T, Van den Berg E, Molenaar WM. Myxofibrosarcoma. In: Fletcher CDM, Unni KK, Mertens F (eds). WHO classification of tumours-Pathology and genetics, tumors of soft tissue and bone. Lyon: IARC Press, 2002; 102-3.
- Huang H, Lal P, Qin J, et al. Low-Grade Myxofibrosarcoma: a clinicopathologic analysis of 49 cases treated at a single institution with simultaneous assessment of the efficacy of 3-tier and 4-tier grading systems. Human Pathology May 2004; 35: 612-21. [?zet]
- Angervall L, Kindblom LG, Merck C. Myxofibrosarcoma. A study of 30 cases. Acta Pathol Microbiol Scand A 1977; 85: 127-40. [?zet]
- Mentzel T, Calonje E, Wadden C, et al. Myxofibrosarcoma: clinicopathologic analysis of 75 cases with emphasis on the low grade variant. Am J Surg Pathol 1996; 20: 391-405. [?zet]
- Graadt van Roggen J, Hogendoorn P, Fletcher C. Myxoid tumours of soft tissue. Histopathology 1999; 35: 291-312. [?zet]
- Fuj?mura T, Okuyama R, Terui T, et al. Myxofibrosarcoma (myxoid malignant fibrous histiocytoma) showing cutaneous presentation: report of two cases. J Cutan Pathol 2005; 32: 512-5. [?zet]
- Merck C, Angervall L, Kindblom LG, Oden A. Myxofibrosarcoma. A malignant soft tissue tumor of fibroblastic-histiocytic origin. A clinicopathologic and prognostik study of 110 cases using multivariate analysis. Acta Pathol Microbiol Immunol Scand Suppl 1983; 282: 1-40.
- Lin CN, Chou SC, Li CF, et al. Prognostic factors of myxofibrosarcomas: implications of margin status, tumor necrosis, and mitotic rate on survival. J Surg Oncol 2006; 93: 294-303. [?zet]
Yaz??ma Adresi (Address for Correspondence):
Dr. Elif TANRIVERD?O,
?ve?ler 2. Cadde 183. Sokak No: 4/9
06460 ANKARA - TURKEY
e-mail: dr.elif06@mynet.com