Sarkoidozlu
olgularda klinik g?r?n?m ve tan?sal yakla??m:
T?rk olgu serisi (sarkoidoz
klini?i ve tan? yakla??mlar?)
G?ksel KITER1, Benan M?SELL?M2,
Erdo?an ?ET?NKAYA3, Hatice T?RKER4, A. Esra KUNT UZASLAN5,
Esin YENT?RK3, O?uz UZUN6, Leyla SA?LAM7,
?zlem ?ZDEM?R KUMBASAR8, G?khan ?EL?K8,
G?lfer OKUMU?9,
Peri Meram ARBAK10, G?ndeniz ALTIAY11, Levent TABAK9,
Ay??n ?AKAR CO?KUN12,
Serdar ERTURAN2, Haluk T?RKTA?13,
Enver YALNIZ14, Atila AKKO?LU15, Candan ????16,
?mer Tamer DO?AN17, Metin ?ZKAN18, Serir ?ZKAN14,
Fatma I??l UZEL19, G?l ?NGEN2
T?rk Toraks Derne?inin Sakroidoz ?al??ma Grubu
1 Pamukkale ?niversitesi T?pFak?ltesi, G???s Hastal?klar? Anabilim Dal?, Denizli,
2 ?stanbul ?niversitesi Cerrahpa?a T?pFak?ltesi, G???s Hastal?klar? Anabilim Dal?, ?stanbul,
3 SB Yedikule G???s Hastal?klar? ve G???s Cerrahisi E?itim ve Ara?t?rma Hastanesi, Solunum Hastal?klar? B?l?m?, ?stanbul,
4 SB S?reyyapa?a G???s Hastal?klar? ve G???s Cerrahisi E?itim ve Ara?t?rma Hastanesi, Solunum Hastal?klar? B?l?m?,?stanbul,
5 Uluda? ?niversitesi T?pFak?ltesi, G???s Hastal?klar? Anabilim Dal?, Bursa,
6 Ondokuz May?s ?niversitesi T?pFak?ltesi, G???s Hastal?klar? Anabilim Dal?, Samsun,
7 Atat?rk ?niversitesi T?pFak?ltesi, G???s Hastal?klar? Anabilim Dal?, Erzurum,
8 Ankara ?niversitesi T?pFak?ltesi, G???s Hastal?klar? Anabilim Dal?, Ankara,
9 ?stanbul ?niversitesi ?stanbul T?pFak?ltesi, G???s Hastal?klar? Anabilim Dal?, ?stanbul,
10 D?zce ?niversitesi T?pFak?ltesi, G???s Hastal?klar? Anabilim Dal?, D?zce,
11 Trakya ?niversitesi T?pFak?ltesi, G???s Hastal?klar? Anabilim Dal?, Edirne,
12 Celal Bayar ?niversitesi T?pFak?ltesi, G???s Hastal?klar? Anabilim Dal?, Manisa,
13 Gazi ?niversitesi T?pFak?ltesi, G???s Hastal?klar? Anabilim Dal?, Ankara,
14 ?zmir Dr. Suat Seren G???s Hastal?klar? ve Cerrahisi E?itim ve Ara?t?rma Hastanesi, G???s Hastal?klar? B?l?m?, ?zmir,
15 Dokuz Eyl?l ?niversitesi T?pFak?ltesi, G???s Hastal?klar? Anabilim Dal?, ?zmir,
16 Akdeniz ?niversitesi T?pFak?ltesi, G???s Hastal?klar? Anabilim Dal?, Antalya,
17 Cumhuriyet ?niversitesi T?pFak?ltesi, G???s Hastal?klar? Anabilim Dal?, Sivas,
18 G?lhane Askeri T?p Fak?ltesi, G???s Hastal?klar? Anabilim Dal?, Ankara,
19 ?stanbul Vatan Hastanesi, ?stanbul.
?ZET
Sarkoidozlu olgularda klinik g?r?n?m ve tan?sal yakla??m: T?rk olgu serisi (sarkoidoz klini?i ve tan? yakla??mlar?)
Sarkoidoz, idiyopatik gran?lomat?z bir hastal?kt?r. Genellikle akci?er tutulumu vard?r. Tan?s?, gran?lomat?z inflamasyonun bilinen di?er nedenlerinin d??lanmas? gereklili?i y?z?nden zor olabilir. ?ok merkezli ?al??mam?zda sarkoidozun klinik g?r?n?mleri ve tan?sal yakla??mlar?n?n de?erlendirilmesi ama?land?. ?al??ma protokol? internet ?zerinden ara?t?rmac?lara g?nderildi ve yeni tan? alm?? sarkoidoz olgular?na ait bilgilerini g?ndermeleri istendi (klinik, radyolojik ve tan?sal). ?ki y?l i?inde 293 hasta verisi topland?. Solunumsal yak?nmalar, hastalar?n %73.3??nde bulundu ve ?ks?r?k en s?k yak?nmayd? (%53.2), dispne (%40.3) ikinci s?kl?ktayd?. Konstit?syonel yak?nmalar hastalar?n yar?s?nda g?r?ld?. En s?k olan? yorgunluktu (%38.6). En yayg?n bulgu eritema nodozum (%17.1) idi. En s?k akci?er radyogram? bulgusu bilateral hiler lenfadenomegali (%78.8) idi. Radyolojik evrelemede hastalar?n ?o?unlu?unun Evre I ve Evre II oldu?u bulundu (s?ras?yla %51.9 ve %31.7). Histolojik do?rulama 265 (%90.4) hastada ger?ekle?mi?ti. Bronkoskopilerin ??te biri normal iken, mukozal hiperemi (%19.8) ve bron? duvar?n?n d??ar?dan bas?s? (%16.8) yayg?n anormal bulgular idi. S?k kullan?lan ?rnekleme y?ntemleri aras?nda yer alan mediastinoskopide tan? ba?ar?s? %100 idi. En s?k kullan?lan tan? y?ntemi olan transbron?iyal biyopsinin ba?ar? oran? %48.8 idi. Sarkoidoza ?ok y?nl? yakla??m, s?k ve seyrek rastlanan bulgular? g?z ?n?nde bulundurularak ay?r?c? tan? listelerinde yer almas?, olas? tutulmu? alanlara y?nelik tan?sal incelemelerin organizasyonu ve birarada ?al??an ekip ?yelerinin konunun uzman? olmas? sayesinde iyile?tirilir.
Anahtar Kelimeler: Sarkoidoz, akci?er, tan?.
SUMMARY
Clinical
presentations and diagnostic work-up in sarcoidosis:
a series of Turkish cases (clinics and diagnosis of sarcoidosis)
G?ksel KITER1, Benan M?SELL?M2,
Erdo?an ?ET?NKAYA3, Hatice T?RKER4, A. Esra KUNT UZASLAN5,
Esin YENT?RK3, O?uz UZUN6, Leyla SA?LAM7,
?zlem ?ZDEM?R KUMBASAR8, G?khan ?EL?K8,
G?lfer OKUMU?9, Peri Meram ARBAK10, G?ndeniz ALTIAY11,
Levent TABAK9, Ay??n ?AKAR CO?KUN12, Serdar ERTURAN2,
Haluk T?RKTA?13, Enver YALNIZ14, Atila AKKO?LU15,
Candan ????16,
?mer Tamer DO?AN17, Metin ?ZKAN18, Serir ?ZKAN14,
Fatma I??l UZEL19, G?l ?NGEN2
Sarcoidosis Working Group of Turkish Thoracic Society
1 Department of Chest Diseases, Faculty of Medicine, Pamukkale University, Denizli, Turkey,
2 Department of Chest Diseases, Faculty of Cerrahpasa Medicine, Istanbul University, Istanbul, Turkey,
3 Department of Chest Diseases, Yedikule Chest Diseases and Chest Surgery Training and Research Hospital, Istanbul, Turkey,
4 Department of Chest Diseases, Sureyyapasa Chest Diseases and Chest Surgery Training and Research Hospital, Istanbul, Turkey,
5 Department of Chest Diseases, Faculty of Medicine, Uludag University, Bursa, Turkey,
6 Department of Chest Diseases, Faculty of Medicine, Ondokuz Mayis University, Samsun, Turkey,
7 Department of Chest Diseases, Faculty of Medicine, Ataturk University, Erzurum, Turkey,
8 Department of Chest Diseases, Faculty of Medicine, Ankara University, Ankara, Turkey,
9 Department of Chest Diseases, Faculty of Istanbul Medicine, Istanbul University, Istanbul, Turkey,
10 Department of Chest Diseases, Faculty of Medicine, Duzce University, Duzce, Turkey,
11 Department of Chest Diseases, Faculty of Medicine, Trakya University, Edirne, Turkey,
12 Department of Chest Diseases, Faculty of Medicine, Celal Bayar University, Manisa, Turkey,
13 Department of Chest Diseases, Faculty of Medicine, Gazi University, Ankara, Turkey,
14 Department of Chest Diseases, Izmir Dr. Suat Seren Chest Diseases and Chest Surgery Training and Research Hospital, Izmir, Turkey,
15 Department of Chest Diseases, Faculty of Medicine, Dokuz Eylul University, Izmir, Turkey,
16 Department of Chest Diseases, Faculty of Medicine, Akdeniz University, Antalya, Turkey,
17 Department of Chest Diseases, Faculty of Medicine, Cumhuriyet University, Sivas, Turkey,
18 Department of Chest Diseases, Gulhane Military Medical Academy, Ankara, Turkey,
19 Istanbul Vatan Hospital, Istanbul, Turkey.
Sarcoidosis is an idiopathic granulomatous disease. It usually affects the lung. The diagnosis may be problematic since the known causes of granulomatous inflammation must be excluded. This multicenter study aimed to evaluate the clinical presentations and diagnostic approaches of sarcoidosis. The study protocol was sent via internet, and the participants were asked to send the information (clinical, radiological and diagnostic) on newly diagnosed sarcoidosis cases. 293 patients were enrolled within two years. Pulmonary symptoms were found in 73.3% of the patients, and cough was the most common one (53.2%), followed by dyspnea (40.3%). Constitutional symptoms were occured in half of the patients. The most common one was fatigue (38.6%). The most common physical sign was eritema nodosum (17.1%). The most common chest radiograhical sign was bilateral hilar lymphadenomegaly (78.8%). Staging according to chest X-ray has revealed that most of the patients were in Stage I and Stage II (51.9% and 31.7%, respectively). Sarcoidosis was confirmed histopathologically in 265 (90.4%) patients. Although one-third of the bronchoscopy was revealed normal, mucosal hyperemi (19.8%) and external compression of the bronchial wall (16.8%) were common abnormal findings. The 100% success rate was obtained in mediastinoscopy among the frequently used sampling methods. Transbronchial biopsy was the most frequently used method with 48.8% success rate. Considering sarcoidosis with its most common and also rare findings in the differential diagnosis, organizing the related procedures according to the possibly effected areas, and the expertise of the team would favour multimodality diagnosis.
Key Words: Sarcoidosis, sarcoidosis, pulmonary, diagnosis.
Sarcoidosis is an idiopathic multisystem granulomatous disease. Pulmonary manifestation is the most common form of the disease; however sarcoidosis can effect any or more than one organ. The clinical presentation may occur in a large spectrum, from asymptomatic mild disease to life-threatening involvement of heart, brain or kidney. Thus its features vary a lot in the case series.
For an accurate diagnosis of sarcoidosis, the multimodality approach including clinical, radiological, and histopathological evaluation is recommended (1).
The diagnostic work-up is being organized in an order by giving the priority to the most possible localization involved, or by advancing from the noninvasive to invasive methods. Clinical presentation gives clues with symptoms and signs. Radiological appearance is the most useful finding both for distinctive diagnosis and for choosing the site for diagnostic approach. Bronchoscopy is a minimal invasive procedure. It has been intended generally for the non-caseating granulomatous inflammation proven by the biopsy. If the presentation is very characteristic like in L?fgren?s syndrom, histopathological diagnosis might not be required (2).
Since mostly pulmonologists are involved in the diagnostic evaluation of sarcoidosis patients, the awareness of extrapulmonary involvement is very essential during the initial investigations. In ACCESS study, the half of the 736 sarcoidosis patients have been reported that they had concomitant extrathoracic involvement (3). The same study has shown that the prevalence of extrathoracic sarcoidosis varied in different populations. For example, erythema nodosum lesions were seen more common in Europeans (1). Possible clinical presentations even other than intrathoracic involvement should be questionned and investigated in the specific populations.
In the cases who required histopathological confirmation of the sarcoidosis, there are several options of diagnostic methods. For patients with pulmonary symptoms, clinicians have various techniques available to make the diagnosis, including transbronchial needle aspiration, bronchoalveolar lavage (BAL), transbronchial biopsy, open-lung biopsy, and mediastinoscopy (4). Each of these techniques have to be considered according to its advantages and disadvantages.
The frequency, clinical presentation and severity of the disease may vary between the races and different study populations (1,3). The aim of the recent multicentered study was to determine the features of clinical presentations and diagnostic methods used in the Turkish sarcoidosis cases, after presenting the epidemiological data on sarcoidosis in a comprehensive study of the same group (5).
MaterialS and methods
This study was organized and conducted by Turkish Thoracic Society Clinical Problems Study Group. Turkish Thoracic Society (TTS) is the largest national, scientific and educational pulmonology society in Turkey. It has over 2400 members, most of which are chest disease specialists. This study was announced via internet to all members of the TTS. Twenty four investigators dealing especially with Sarcoidosis patients in 19 centers of 12 cities in 6 different regions were attended to the study (5). These investigators were employed in general outpatient clinics of pulmonology departments.
Study protocol and case record forms were sent to investigators via internet. Newly diagnosed cases were recorded to the electronic case record forms which were collected by one of the investigators. Cases newly diagnosed as sarcoidosis between 1st of June 2004 and 31st of May 2006 were enrolled to the study. Formerly diagnosed cases were excluded. According to the study protocol, cases with compatible clinical and radiological findings and with histologically proven non-caseating granulomas were accepted as sarcoidosis after the exclusion of other causes of granulomas such as tuberculosis, hypersensitivity pneumonia, Crohn?s disease, etc. Histological confirmation was not a necessity for patients with classical L?fgren?s syndrome.
In the study population; demographic features, clinical presentation symptoms (initial and overall) and physical examination findings, pulmonary function test (PFT) results, radiological appearance, bronchoscopic findings including endobronchial lesions, bronchoalveolar lavage fluid (BALF) examination, and biopsy results were evaluated.
Chest radiographs were classified by Scadding stages: 0, normal chest radiographic findings; I, bilateral hilar adenopathy with normal lung parenchyma; II, bilateral hilar adenopathy with pulmonary infiltrates; III, pulmonary infiltrates without hilar adenopathy; IV, pulmonary fibrosis/fibrocystic parenchymal changes (1,6).
Statistical analyses were computed by SPSS 13.0 package programme. Data were presented as percentage or median/mean ? standard deviation (SD) as appropriate. Mean age was compared by using student?s t test between female and male patients. The relation with different parameters (age, smoking status, symptoms, physical signs, PFT results and, radiological and bronchoscopic findings), and BALF cell discrimination type was investigated by logistic regression analysis. p values < 0.05 were considered as statistically significant.
Results
Within 2 years 293 patients were enrolled to the study; 198 of them were female (67%), and F/M ratio was 2.08. Mean age of the study population was 44 ? 13 years (minimum: 17, maximum: 90). Mean age of male and female patients were found as 38 ? 12 years and 48 ? 13 years, respectively (p< 0.001).
Previous tuberculosis and extrapulmonary tuberculosis were declared in the medical histories of 5 (1.7%) patients and 2 (%0.7) patients, respectively.
The median diagnosis duration for sarcoidosis was 3 months.
Pulmonary symptoms were found in 73.3% of the patients, while cough was the most common one, followed by dyspnea. Constitutional symptoms were occured in half of the patients. The most common one was fatigue (38.6%). The frequencies of pulmonary and constitutional symptoms were shown in descending order (Table 1). The most common extrapulmonary symptoms were erythema nodosum and joint pain (21.5% and 20.8%, respectively) (Table 2).
Separately considering the initial symptom in detail among pulmonary ones, cough has been complained in 127 (43.3%) patients. Dyspnea and chest pain were the other initial pulmonary symptoms occured in 66 (22.5%) and 23 (7.8%) patients, respectively. The mean duration for pulmonary symptoms was 10 ? 21 months before the diagnosis. There was no pulmonary symptoms as an initial symptom in 77 (26.3%) patients.
Among the extrapulmonary symptoms, most of the patients have complained fatigue as initial symptom (15.4% of all patients). The rest of the initial extrapulmonary symptoms were found as erythema nodosum (10.9%), joint pain (8.9%), skin lesion (8.9%), back pain (7.5%), weight loss (4.8%) and fever (3.1%), and mass in neck (2.4%). Other extrapulmonary initial symptoms were found in a few patients (less than 2%).
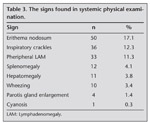
The most common sign in systemic physical examination was eritema nodosum (17.1% of all patients) (Table 3).
Tuberculin skin test (TST) was performed in 227 patients (%77.5). In 152 (67%) of them, the test result was reported as anergic. The enduration measured, and the diameters were reported as between 1-9 mm in 33 patients (14.5%), between 10-14 mm in 23 patients (7.4%), and above 15 mm in 19 patients (6.3%).
Serum angiotensin-converting enzyme (ACE) level was assessed in 179 (61.1%) patients. In 70 (39.1%) of them, the result was higher than upper limit of normal value accepted in each laboratory.
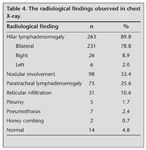
Radiological findings in chest X-rays were determined (Table 4). The most common finding was bilateral hilar lymphadenomegaly (78.8%). In 4.8% of the sarcoidosis patients, the chest radiography was normal. Staging according to chest radiography has revealed that most of the patients were in Stage I and Stage II (51.9% and 31.7%, respectively). The rest of the patients were distributed into Stage 0, Stage III and Stage IV as 4.8%, 5.1% and 0.7% of the patients, respectively.
In 97.6% of the patients, the thoracic CT results were documented. The most common finding was mediastinal lymphadenomegaly, and the detected parenchymal lesions were listed in details (Table 5).
Symptoms and signs characteristic for L?fgren?s Syndrom (erithema nodosum, joint pain, fever and hilar lymphadenomegaly) were found together in 5 (1.7%) patients. All those findings except fever were occured in 11 (3.8%) patients.
PFTs were recorded in 257 patients, and CO difussion test was performed in 161 patients. The FVC, FEV1, FEV1/FVC, MMEF, DLco and DLco/VA parameters were presented as mean ? SD values (Table 6).
The diagnosis was secured with clinical and radiological findings in 28 (9.6%) patients. At the same time, diagnosis was confirmed histopathologically in 265 (90.4%) patients.
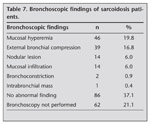
In bronchoscopic evaluation of 231 patients, 37.7% revealed normal appearance. Mucosal hyperemi and external compression of the bronchial wall were the most common abnormal findings (Table 7).
In 79 sarcoidosis patients, the cell discrimination results of BALF was obtained (26.9%). The lymphocytic plus neutrofilic alveolitis was the most common type of alveolitis (46.8%). Lone lymphocytic alveolitis was found in 34.2% of the patients. Lone neutrophilic alveolitis and mixt alveolitis had the same ratio (5.1%), while no alveolitis was found in 8.9% of the sarcoidosis patients. Neutrophilic plus lymphositic alveolitis was found associated with only being recently active smoker (p= 0.03). The age, symptoms, physical signs, PFT results, and radiological and bronchoscopic findings have shown no statistically significant relations with BALF cell discrimination (p> 0.05).
The highest success rate was obtained in mediastinoscopy among the frequently used sampling methods. Transbronchial biopsy was the most frequently used method with 48.8% success rate (Table 8).
Discussion
In the present study, the clinical presentations mostly seen in Turkish sarcoidosis cases were documented. Cough was the most common symptom, even as initial symptom. Fatigue was the most common constitutional symptom. Erythema nodosum has been complained and also found in physical examination frequently. Physical examination findings were not specific for sarcoidosis. Radiologically, hilar lymphadenomegaly was seen frequently and especially in bilateral localization. Most of the patients were in Stage I according to radiological findings. Bronchoscopy has yielded in half of the patients. Lymph node biopsies and other surgical methods had the highest success rates, although they have been used rarely.
Sarcoidosis was seen more common in females in the present study. Although there are studies that reported more than 2 folds (1,3,7) of female dominance, in some of the studies female/male ratio has been found between 1 and 1.8 (8,9).
Study population was consisted of middle-aged patients. At the same time male sarcoidosis patients were younger than females. Same finding has been reported previously in ACCESS study (3). In the series of Reynolds et al., common but possible nonrelated accompanying diseases seen frequently in that age group have been emphasized as possible confronting factor especially in extrapulmonary sarcoidosis diagnosis (10).
There are several other causes of granulomas, including infections such as tuberculosis and fungal infections (3). Other granulomatous diseases must be excluded, although it?s sometimes difficult even with histopathological proof of the ?noncaseating? form of granulomas (1,11). Tuberculosis must be questioned in medical history, and reactivity should be investigated carefully. Among the patients enrolled to the present study, only 7 patients had previous tuberculosis history and none of them had reactivity findings. None of the patients had specific occupational or enviromental exposure history.
Delay in diagnosis might be a problem because of asymptomatic patients and patients with nonspecific symptoms (4,8). Also there may be a time period to be convinced that treatment choices for other pulmonary diseases didn?t work. Judson et al. have found that only 15.3% of the sarcoidosis patients could be diagnosed in first physician visit and more than 20% of the patients had required 6 or more visits until diagnosis was established. Also more than one-fourth of sarcoidosis patients couldn?t be diagnosed within 6 months of initial symptom and 10% patients within 2 years of initial symptoms (8). However, in the present study, the median diagnosis duration was 3 months. That might be related with the high tendency to order chest X-ray as a routine procedure, and the settled diagnostic procedures for the hilar lymphadenomegalies.
Cough, dyspnea and chest pain have been reported in one-third to one-half of the patients and hemopthysis was rarely occured (1,3,4). In the present study, pulmonary symptoms were the most common complaints with the predominancy of cough which was followed by dyspnea. Chest pain was occurred in one-fourth of the patients. There seems the pulmonary presentation of sarcoidosis has same features in different populations.
Extrapulmonary symptoms may occur alone or together with pulmonary symptoms. In the present study, erythema nodosum and joint pain were the most common extrapulmonary symptoms which were followed by back pain. Although not required in all cases, skin lesions as erythema nodosum and lupus pernio are important for diagnosing sarcoidosis since they are very characteristic and when intended, biopsy sampling could be performed easily. Mert et al. have been reported 10% of the erythema nodosum patients had sarcoidosis among the wide spectrum of other diseases (12). ACCESS study has presented that %8.2 of the patients had erythema nodosum (3). In the present study, erythema nodosum was occured in one-fourth of patients, while no lupus pernio was mentioned except nonspecific definition as skin lesion in 16% of patients. The diagnosis was made by skin biopsy in 10% of all patients.
Back pain was also seen in the same frequency of skin lesions (16%). That extrapulmonary symptom has been reported in sporadic case reports as a rare symptom or presentation of sarcoidosis (13). Even back pain has been complained frequently, only a few of those patients had pathological findings of sacroiliitis might be related with sarcoidosis (14). Back pain as being a nonspecific and subjective symptom is hard to related with sarcoidosis.
Although nonspecific constitutional symptoms such as fatigue, fever, weight loss have been reported as observable in one-third of the sarcoidosis patients (1), half of the patients had those symptoms in the present study. Among the constitutional symptoms, fatigue was the most common one. Fatigue and unexplained fever might get the attention to sarcoidosis (15).
In the study of Judson et al., initial symptoms have been found in half of the patients (half of them were only pulmonary) and skin lesions were reported in 12.7% as the initial symptom. Constitutional symptoms have been reported only in 6.3% of the patients (8). In the present study, there was no pulmonary symptoms at the beginning in 26.3% of the patients. Although the ratio of having pulmonary or extrapulmonary symptoms as presenting symptom were similar, in 16.7% of the patients the combination was occured. Consultating the patients in suspicion of sarcoidosis, even without pulmonary symptoms, with a chest disease specialist might help to detect the asymptomatic pulmonary involvement.
A negative TST in the general population is a sensitive test for sarcoidosis. A positive TST among sarcoidosis patients have been suggested for indicating tuberculosis (16). In the present sudy, most of the patients had anergic or negative TST results, and in all of the TST positive patients tuberculosis has been excluded.
Certain laboratory tests, such as serum Angiotensin-converting enzyme level, while often helpful in corroborating the diagnosis, did not make the diagnosis of sarcoidosis definitive (10). In the present study, high serum ACE levels were detected only in 40% of the patients who had serum ACE testing (61% of all).
Bilateral hilar adenopathy, or bilateral hilar adenopathy accompanied by characteristic findings of sarcoidosis, ie, uveitis, arthritis, or erythema nodosum, as ?clinically evocative of sarcoidosis,? have been conservatively estimated and observation has been recommended over biopsy confirmation (1,4,10). In 90% of the patients had hilar lymphadenopathy; mostly in bilateral localization. Nodular involvement was seen in one-third of the patients. The number of patients with normal chest radiography was low, and being investigated in pulmonary clinics might be a possible explaination for that result.
Although sarcoidosis can involve any organ, it affects the lungs in 90% of patients (15). Stage I and II sarcoidosis have been reported as the most frequent forms in many studies similar to the present study (3,7).
Computed tomography (CT) of the chest is not routinely necessary, high-resolution CT is indicated in approximately 30% of patients with the presence of atypical clinical and/or chest radiographical findings and suspected complications of other lung diseases (15). In the present study, only in 2.4% of the patients CT was not performed. Even for the severe pulmonary sarcoidosis patients, CT scan is the most accurate technique to thoroughly assess the complications: it allows to detect them, to make clear their underlying mechanisms and subsequently to help the clinicians in their approach to the therapy and the prognosis of patients (17). In the present study, the most common CT appearance was mediastinal lymphadenomegaly, followed by nodules and reticular infiltrations. The low frequency of diffuse fibrosis and honey combing was consisted with very low frequency of Stage IV sarcoidosis patients. In the absence of fibrosis, localized bronchiectasis may rarely develop downstream from a bronchial obstruction, secondary to either endobronchial sarcoid or extrinsic compression by enlarged nodes (17). The 3% ratio for bronchiectases may reflect that the less severe forms of disease had the predominancy in the recent series of sarcoidosis.
With the introduction of CT scan, especially high-resolution CT, awareness of pleural manifestations of sarcoidosis has increased, allowing detection of more subtle cases of pleural involvement, a rare (with 2-4% frequency) but significant involvement (18). The rates were similar in the present study, however, pleural calsification reported among the CT findings was conspicuous. It might be a co-incidence with asbestos exposure, or a sequel of previous tuberculosis pleuresy.
In ACCESS study, more than 30% of the patients had restrictive disease and 14% of patients had obstructive disease (3). Similar findings have been reported in another study (7). In a large study of German and Swiss patients, more than 20% of patients at initial diagnosis had restrictive disease (10). In the present study, since the mean values of the pulmonary functions were normal, the patients with restrictive defect (FVC < 75%) was found in 19.9%.
Pulmonary diffusion impairment have been reported in 50% of the sarcoidosis patients (7). In the recent study, 34.5% of the patients were reported as having DLco below 75% predicted.
In sarcoidosis, confirmation of the characteristic non-caseating granulomas in appropriate biopsy specimen are generally required (1,19). The choice of the site to be biopsied differs according to the clinical and radiological clues for possibly involved tissues/organs, the oppurtunities and experience of the team (physician, surgeon and pathologist) and patient?s health status. In the present study, biopsy confirmation via different procedures was achieved in 90% of the patients.
Bronchoscopy is a safe and minimal invasive procedure which provides many options for getting cells, and tissues to be examined. For patients with pulmonary symptoms, clinicians have various techniques available to make the diagnosis, including needle aspiration, BAL, transbronchial biopsy, open-lung biopsy, and mediastinoscopy (4). Each of these techniques has advantages and disadvantages.
BAL is safe, minimally invasive, and provides useful information for the diagnosis of sarcoidosis. The characteristic findings in BAL for sarcoidosis are a normal or only mildly elevated total cell count with a predominance of lymphocytes, usually a normal percentage of eosinophils and neutrophils, and an absence of plasma cells and foamy alveolar macrophages (15). The cell discrimination findings of BALF in the present study were revealed the predominancy of lymphocytic plus neutrophilic and lone lymphocytic alveolitis. Since the standardization of the technique is very important to interpret those findings accurately, that result must be interpretted cautiously. However, being recently active cigarette smoker had a statistical significant relation with having increased amount of neutrophils in BALF. Smoking is a well known factor for increased neutrophil amount in BALF. Disease presentation or activity at the time the BAL is performed, as well as the smoking status is crucial for interpretation of individual BALF analysis results (20).
Sarcoid granulomas can involve any aspect of the respiratory tract. Endobronchial abnormalities are commonly observed in patients with sarcoidosis (21). No abnormal finding was documented in 37.1% of the patients in the present study. The normal appearance of mucosa during bronchoscopy should not be the reason to avoid taking biopsies. Bjermer et al. have reported that biopsies taken from normal-appearing mucosa parts have revealed 35.6% positive results for sarcoidosis and in 70.6% of the patients with swollen endobronchial mucosa, the biopsies were positive (20). The diagnostic yield of endobronchial biopsy (EBB) in sarcoidosis have been reported as high, even when the mucosa appeared normal (21-23). Since the number of patients with abnormal broncoscopic appearance was higher than the number of patients whose bronchial mucosa biopsy was taken, it might be considered that there was not any inclination to biopsy the normal mucosa randomly. However, in the present study, one-third of the patients had EBB and half of them were diagnostic. The ratio has been report in series as 45%, 50% and 68% in Stage I, II and III sarcoidosis respectively and adding EBB to TBLB have been shown to increase the diagostic yield of TBLB (24).
Transbronchial lung biopsy (TBLB) is one of the preferred diagnostic methods for pulmonary sarcoidosis with a wide range of diagnostic accuracy (1). TBLB has become the accepted standard of care in all patients with suspected sarcoidosis despite variances in radiographic stage and disease activity (by considering factors affecting diagnostic yield of the technique) (23). In the present study, TBLB was performed in 43% of the patients and half of them were diagnostic.
Transbronchial needle aspiration biopsy is the less invasive method to get biopsy from the lymph nodes. However, interpretting cytology specimen needs more expertise. In the study of Cetinkaya et al., diagnostic yield of TBNA in the patients with adequate lymph node tissue was obtained have been reported as 87% including fewer tuberculosis and malignency patients (25). In the present study, the diagnostic yield of TBNA biosy was the lowest among the biopsy techniques. Since the cases were evaluated in different centers, the reason might be the difference in the expertise of that technique.
One of the invasive methods to obtain tissue for diagnosing sarcoidosis is mediastinoscopy (4,19). The published literature may underestimate the morbidity/mortality of this procedure, which is highly dependent on the experience and skill of the operator, possibly due to the reports of institutions with large and favorable experiences. In a meta-analysis, it is been found that total complications were ranged from 1.4 to 2.3% (2). In the present study, one-third of the patients had diagnosed via mediastinoscopy with 100% diagnostic success rate. Possibly, need for general anesthesia and expertise of the surgeon might cause the avoidance of that technique to get biopsy. The advantage of mediastinoscopy have been addressed as its particular usefulness in distinguishing between sarcoidosis and lymphoma (4).
The invasive methods as lymph node biopsies (scalen or peripheral), mediastinotomy, open or VATS lung biopsy are expecting higher diagnostic yields like in the present study. After all, morbidity/mortality rates need to be considered seperately as well as cost-effectiveness. Baughman has suggested mediastinoscopy for significant adenopathy and VATS for minimal adenopaty (4). Open-lung biopsy, usually performed by video-assisted thoracoscopy, is associated with significant morbidity (4). The major reason for choosing this procedure is the clinician?s concern about other interstitial lung diseases, such as idiopathic pulmonary fibrosis. In a prospective study of patients undergoing serial evaluations and eventual open-lung biopsy for idiopathic interstitial lung disease, 3 of 91 were found to have sarcoidosis (6).
In conclusion; sarcoidosis is an unique and challenging disease with its clinical presentations, and diagnostic work-up. Considering sarcoidosis with its most common and also rare findings in the differential diagnosis, organizing the related procedures according to the possibly effected areas, and expertise of the team would favour multimodality diagnosis.
Conflict of interest
Neither author has a financial relationship with a commercial entity that has an interest in the subject of this manuscript.
REFERENCES
- Statement on sarcoidosis. Joint Statement of the American Thoracic Society (ATS), the European Respiratory Society (ERS) and the World Association of Sarcoidosis and Other Granulomatous Disorders (WASOG) adopted by the ATS Board of Directors and by the ERS Executive Committee, February 1999. Am J Respir Crit Care Med 1999; 160: 736-55. [Tam Metin] [PDF]
- Reich JM, Brouns MC, O?Connor E, Edwards MJ. Mediastinoscopy in patients with presumptive stage I sarcoidosis: a risk/benefit, cost/benefit analysis. Chest 1998; 113: 147-53. [?zet] [PDF]
- Baughman RP, Teirstein AS, Judson MA, Rossman MD, Yeager H Jr, Bresnitz EA, et al.; Case Control Etiologic Study of Sarcoidosis (ACCESS) Research Group. Clinical characteristics of patients in a case control study of sarcoidosis. Am J Respir Crit Care Med 2001; 164: 1885-9. [?zet] [Tam Metin] [PDF]
- Baughman RP. Pulmonary sarcoidosis. Clin Chest Med 2004; 25: 521-30. [?zet]
- Musellim B, Kumbasar OO, Ongen G, Cetinkaya E, Turker H, Uzaslan E, et al. Epidemiological features of Turkish patients with sarcoidosis. Respir Med 2009; 103: 907-12. [?zet]
- Hunninghake GW, Costabel U, Ando M, Baughman R, Cordier JF, du Bois R, et al. Statement on sarcoidosis (the joint statement of the American Thoracic Society, the European Respiratory Society, and the World Asoociation of Sarcoidosis and Other Granulomatous Disorders). Am J Respir Crit Care Med 1999; 160: 736-55.
- Mihailovic-Vucinic V, Zugic V, Videnovic-Ivanov J. New observations on pulmonary function changes in sarcoidosis. Curr Opin Pulm Med 2003; 9: 436-41. [?zet]
- Judson MA, Thompson BW, Rabin DL, Steimel J, Knattereud GL, Lackland DT, et al. The Diagnostic Pathway to Sarcoidosis. Chest 2003; 123: 406-12. [?zet] [Tam Metin] [PDF]
- Loddenkemper R, Kloppenborg A, Schoenfeld N, Grosser H, Costabel U. Clinical findings in 715 patients with newly detected pulmonary sarcoidosis: results of a cooperative study in former West Germany and Switzerland. WATL Study Group: Wissenschaftliche Arbeitsgemeinschaft f?r die Therapie von Lungenkrankheiten. Sarcoidosis Vasc Diffuse Lung Dis 1998; 15: 178-82. [?zet]
- Reynolds HY. Sarcoidosis: impact of other illnesses on the presentation and management of multi-organ disease. Lung 2002; 180: 281-99. [?zet]
- Okumus G. The Diagnosis and Differential Diagnosis in Sarcoidosis. Turkiye Klinikleri J Pulm Med-Special Topics 2009; 2: 44-50
- Mert A, Kumbasar H, Ozaras R, Erten S, Tasli L, Tabak F, et al. Erythema nodosum: an evaluation of 100 cases. Clin Exp Rheumatol 2007; 25: 563-70. [?zet]
- Morgan SS, Aslam MB, Mukkanna KS, Ampat G. A rare presentation of sarcoidosis, back pain and spondylolisthesis. J Bone Joint Surg Br 2008; 90: 240-2. [?zet]
- Erb N, Cushley MJ, Kassimos DG, Shave RM, Kitas GD. An assessment of back pain and the prevalence of sacroilitis in sarcoidosis. Chest 2005; 127: 192-6. [?zet] [Tam Metin] [PDF]
- Costabel U, Ohshimo S, Guzman J. Diagnosis of sarcoidosis. Curr Opin Pulm Med 2008; 14: 455-61. [?zet]
- Smith-Rohrberg D, Sharma SK. Tuberculin skin test among pulmonary sarcoidosis patients with and without tuberculosis: its utility for the screening of the two conditions in tuberculosis-endemic regions. Sarcoidosis Vasc Diffuse Lung Dis 2006; 23: 130-4. [?zet]
- Hennebicque AS, Nunes H, Brillet PY, Moulahi H, Valeyre D, Brauner MW. CT findings in severe thoracic sarcoidosis. Eur Radiol 2005; 15: 23-30. [?zet]
- Mihailovic-Vucinic V, Jovanovic D. Pulmonary sarcoidosis. Clin Chest Med 2008; 29: 459-73. [?zet]
- Ece T. Invasive diagnosis of sarcoidosis. Turkiye Klinikleri J Pulm Med-Special Topics 2009; 2: 68-71.
- Drent M, Mansour K, Linssen C. Bronchoalveolar lavage in sarcoidosis. Semin Respir Crit Care Med 2007; 28: 486-95. [?zet]
- Torrington KG, Shorr AF, Parker JW. Endobronchial disease and racial differences in pulmonary sarcoidosis. Chest 1997; 111: 619-22. [?zet] [PDF]
- Bjermer L, Thunell M, Rosenhall L, Stjernberg N. Endobronchial biopsy positive sarcoidosis: relation to bronchoalveolar lavage and course of disease. Respir Med 1991; 85: 229-34. [?zet]
- Chapman TJ, Mehta AC. Bronchoscopy in sarcoidosis: diagnostic and therapeutic interventions. Curr Opin Pulm Med 2003; 9: 402-7. [?zet]
- Bilaceroglu, Perim K, Gunel O, Cagirici U, Buyuksirin M. Combining transbronchial aspiration with endobronchial and transbronchial biopsy in sarcoidosis. Monaldi Arch Chest Dis 1999; 54: 217-23. [?zet]
- Cetinkaya E, Yildiz P, Kadakal F, Tekin A, Soysal F, Elibol S, et al. Transbronchial needle aspiration in the diagnosis of intrathoracic lymphadenopathy. Respiration 2002; 69: 335-8. [?zet]
Yaz??ma Adresi (Address for Correspondence):
Dr. G?ksel KITER,
Pamukkale ?niversitesi T?p Fak?ltesi,
G???s Hastal?klar? Anabilim Dal?,
DEN?ZL? - TURKEY
e-mail: gokselkiter@yahoo.com