Bronkoskopik inceleme ile tan? alan endobron?iyal t?berk?loz olgusu
Yasemin SAYGIDE?ER, Burcu OKTAY, Emine SEVG?, ?zlem SEVER, Hikmet FIRAT, Sad?k ARDI?
SB D??kap? Y?ld?r?m Beyaz?t E?itim ve Ara?t?rma Hastanesi, G???s Hastal?klar? Klini?i, Ankara.
?ZET
Bronkoskopik inceleme ile tan? alan endobron?iyal t?berk?loz olgusu
Endobron?iyal t?berk?loz (EBTB), trakeobron?iyal a?ac?n t?berk?loz ile infeksiyonu olarak tan?mlan?r ve eri?kin pop?lasyonda s?k rastlanmayan bir durumdur. Parankimal hastal?k g?r?lmedi?inde EBTB daha az fark edilmekte ve tan?da zorluklara neden olmaktad?r. Amac?m?z, az g?r?len ve seyri s?ras?nda bronkostenoz geli?ebilmesi a??s?ndan ?nemli olan bu hastal?kla ilgili bir olguyu sunmakt?r. Olgudaki, 20 ya??ndaki kad?n hasta iki ayd?r nonprod?ktif ?ks?r?k, nefes darl??? ve son d?nemde minimal hemoptizi ile ba?vurmu?tur. Klinik ve radyolojik de?erlendirme sonras?nda fleksibl bronkoskopi ile ana karinadan itibaren her iki ana bron?ta ?ok say?da t?m?r g?r?n?ml? endobron?iyal lezyon izlenmi?tir. Biyopsi sonras? tan? EBTB gelmi? ve antit?berk?loz tedavinin ikinci ay?nda endobron?iyal lezyonlar kaybolmu?tur. Hasta stenoz geli?meden iyile?mi?tir. Bu olgu, endobron?iyal lezyonlar?n ay?r?c? tan?s?nda EBTB?nin de akla gelmesi gereklili?ini hat?rlatmaktad?r. EBTB olgular?n?n komplikasyonsuz iyile?ebilmesi zaman?nda tan? ve tedavi ba?lanmas? ile olanakl?d?r.
Anahtar Kelimeler: Endobron?iyal t?berk?loz, bronkoskopi, endobron?iyal kitle.
SUMMARY
Bilateral multiple tumor-like endobronchial tuberculosis, diagnosed with bronchoscopic examination
Yasemin SAYGIDE?ER, Burcu OKTAY, Emine SEVG?, ?zlem SEVER, Hikmet FIRAT, Sad?k ARDI?
Department of Chest Diseases, Diskapi Yildirim Beyazit Training and Research Hospital, Ankara, Turkey.
Endobronchial tuberculosis is defined as tuberculosis infection of tracheobronchial tree and it is not seen often in adult population. In the absence of parenchymal disease endobronchial tuberculosis is less well-recognized and can lead to difficulties in diagnosis. Our aim is to introduce a rare form of tuberculosis that is important because of high probability of developing severe bronchostenosis during its course. We report a 20-year-old woman who presented with two-month history of severe non-productive cough, shortness of breath, and hemoptysis. After clinical and radiological evaluation, flexible bronchoscopy showed bilateral multiple tumorous lesions that were seen from main carina down to the both main bronchus. The biopsy samples revealed EBTB diagnosis and antituberculosis therapy was given. At the second month of the therapy, rebronchoscopy revealed almost disappearance of the polypoid lesions. The patient healed without any stenosis. This case report is a reminder that endobronchial tuberculosis must take into consideration in differential diagnosis of endobronchial lesions. In patients with endobronchial tuberculosis healing without any complication could be achieved with timely diagnosis and commencement of early treatment.
Key Words: Endobronchial tuberculosis, bronchoscopy, endobronchial mass.
Although endobronchial tuberculosis is a rare condition in adult population, it continuous to be a health problem because of having a high incidence of positive sputum samples and high probability of developing severe bronchostenosis? during its course (1,2). It is often misdiagnosed as bronchial asthma and lung cancer (3,4,5). Misdiagnose of the disease leads to increase public health concern. Endobronchial tuberculosis is usually thought to be associated with pulmonary tuberculosis (6). However it could be occur in the absence of parenchymal infiltration as well (4).? Early diagnosis and early administration of antituberculosis chemotherapy before involvement of the deeper airways is important to prevent the development of bronchostenosis (7). We report a patient with endobronchial tuberculosis who had no parenchymal infiltration and healed without bronchostenosis.
CASE REPORT
A 20-year-old woman presented with a two-month history of severe non-productive cough, shortness of breath and wheezing. She had noted difficulty in swallowing and described a small amount of fresh blood came after a strong and severe chough for once, one week before she referred to our clinic. She had no history of bronchial asthma, previous chronic disease and had never smoked.? She did not complain of weight loss, fever and night sweats. She had given non-specific oral antibiotics and inhaler form of bronchodilators without any improvement. She reported deterioration in her symptoms during previous one month. On physical examination her vital signs were stable. There was no lymphadenopathy, enlargement of liver or spleen. Auscultation of the chest was normal. No rale, rhoncus and cardiac murmur was detected. Her erythrocyte sedimentation rate was 56 mm/hour. Serum hemoglobin level was 9.6 g/dL, total white blood cell count was 9.10 x 109/L. Lymphocytes were 17.2%, platelets were 405 x 109/L. Spirometric examination was normal. She could not obtain available sputum sample for the examination of acid-fast bacilli.
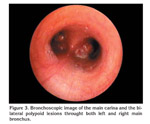
The chest radiograph showed a prominent left hilum with no infiltration on the lung parenchyma (Figure 1). The chest computed tomography demonstrated a polyploid figure in the left main bronchus and a figure of mass on the upper part of the left hilum (Figure 2). After her clinical history and chest computed tomography scan were evaluated, we decided to carry out flexible bronchoscopic examination with the suspicious of malignancy and endobronchial tuberculosis. Flexible bronchoscopy showed bilateral multiple tumorous lesions that were seen from main carina down to the both main bronchus (Figure 3,4). The mucosa was mildly hyperemic and minimal edematous. The mucosal punch biopsies were obtained from the endobronchial tumorous lesions. Histopathologic examination revealed granulomatous inflammation without caseification, but compatible with tuberculosis. Special stains showed no acid-fast bacilli and no malignant cells. On the basis of clinical, radiologic and histopathologic findings, anti-tuberculosis therapy initiated. The patient was treated with isoniazid, rifampicin, morphzinamid and ethambutol. Neither oral nor inhaler corticosteroid was given.
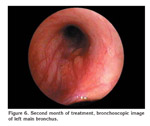
The culture of bronchial lavage at four weeks was reported negative for tuberculosis. She reported resolution of her symptoms after one month of therapy. At the second month of the therapy, rebronchoscopy revealed almost disappearance of the tumorous lesions (Figure 5,6). Therapy was prolonged for six months with isoniazid and rifampycin. The patient healed successfully without bronchostenosis.
DISCUSSION
Endobronchial tuberculosis is known as a very infectious form of tuberculosis that remains a diagnostic challenge (8). It is usually seen at the younger population, and female predominance (3). The pathogenesis of endobronchial tuberculosis is not yet fully established. However, proposed mechanisms include direct implantation of tubercle bacilli into the broncus from an adjacent pulmonary parenchymal lesion, direct airway infiltration from an adjacent tuberculous mediastinal lymph node, erosion and protrusion of an intrathoracic tuberculous lymph node into bronchus, hematogenous spread, and extension to the peribronchial region by lymphatic drainage (2,3,9).?
Clinical manifestations of endobronchial tuberculosis are non-specific and include chronic productive cough, barking cough, chest pain, haemoptysis, generalized weakness, dyspnoea and fever (10). 10% to 20% of patients with endobronchial tuberculosis may have normal chest radiographs. Because of these reasons diagnose is often delayed and/or patients are misdiagnosed as bronchial asthma and malignancy (4). Delayed diagnose leads to delayed treatment which is associated with increased complication rate and public health concern (7). The most important goals of the treatment in endobronchial tuberculosis are the eradication of tubercle bacilli and prevention of bronchial stenosis (11). Bronchial stricture could develop in 60-95% of cases (12,13). Computed tomography is very useful in evaluating endobronchial lesions such as obstruction and stenosis (14). In our case, endobronchial tumorous lesions were detected by computed tomography. At this point it is important to take into consideration endobronchial tuberculosis in the differential diagnosis of endobronchial lesions. The bronchoscophic approach is mandatory to prompt diagnosis of endobronchial tuberculosis (15,16). Chung and Lee, described the bronchoscopic features of endobronchial tuberculosis and classified it into seven subtypes as;
1. Actively caseating,
2. Oedematous-hyperaemic,
3. Fibrostenotic,
4. Tumorous,
5. Granuler,
6. Ulcerative,
7. Non-spesific bronchitic endobronchial tuberculosis. They also defined the therapeutic outcomes of these subtypes (2).
In our case, bilateral, multiple tumorous lesions were seen on bronchoscopic examination. The tumorous lesions were minimally obstructing the bronchus and seemed to not covered with caseous material as opposed to tumorous endobronchial tuberculosis. Only mild mucosal swelling and/or hyperemia were seen on bronchoscopy. Bronchoscopic and computed tomography images of the lesions were simulating malignancy. However tuberculosis was proven by bronchoscopic biopsy of these lesions. At the second month of the therapy, rebronchoscopy revealed the almost disappearance of the tumorous lesions. The prognosis was so excellent. Although mild mucosal swelling and/or hyperemia and good prognosis were compatible with non-spesific bronchitic endobronchial tuberculosis, we did not classified our patient into this type. Because in? our case addition to mild mucosal swelling and/or hyperemia, there were multiple bilateral tumorous lesions on bronchoscophy. According to current classification of endobronchial tuberculosis, our case did not correspond clinically with any of seven types similar to Al-Maslamani?s case, and our case did not show any bronchostenosis similar to Araz?s study (17,18). Considering the recently reported cases it may suggest that future researches are required to create more comprehensive classification of endobronchial tuberculosis.
In conclusion, this case report is a reminder that endobronchial tuberculosis must take into consideration in differential diagnosis of endobronchial lesions. In patients with endobronchial tuberculosis healing without any complication could be achieved with timely diagnosis and commencement of early treatment.
CONFLICT of INTEREST
None declared.
REFERENCES
- Kreisel D, Arora N, Weisenberg S, Saqi A, Krupnick A, Demetriades A, et al. Tuberculosis presenting as an endobronchial mass. J Thorac Cardiovasc Surg 2007; 133: 582-4. [Tam Metin] [PDF]
- Chung H, Lee J. Bronchoscopic assessment of the evolution of endobronchial tuberculosis. Chest 2000; 117: 385-92. [?zet] [Tam Metin] [PDF]
- Lee J, Park S, Lee D, Shin D, Yang S, Yoo B. Endobronchial tuberculosis. Clinical and bronchoscopic features in 121 cases. Chest 1992; 102: 990-4. [?zet] [PDF]
- Lee T, Sin Fai, Lam K. Endobronchial tuberculosis simulating bronchial asthma. Singapore Med J 2004; 45: 390-2. [?zet] [PDF]
- Matthews J, Matarese S, Carpenter J. Endobronchial tuberculosis simulating lung cancer. Chest 1984; 86: 642-4. [?zet] [PDF]
- Hoheisel G, Chan B, Chan C, Chan K, Teschler H, Costabel U. Endobronchial tuberculosis: Diagnostic features and therapeutic outcome. Respir Med 1994; 88: 593-7. [?zet]
- Um S, Yoon Y, Lee S, Yim J, Yoo C, Chung H, et al. Predictors of persistent airway stenosis in patients with endobronchial tuberculosis. Int J Tuberc Lung Dis 2008; 12: 57-62. [?zet]
- Kashyap S, Mohapatra P, Saini V. Endobronchial tuberculosis. Indian J Chest Dis Allied Sci 2003; 45: 247-56. [?zet]
- Kim Y, Kim H, Lee K, Uh S, Cung Y, Park C. Serial fiberoptic bronchoscopic observations of endobronchial tuberculosis before and early after antituberculosis chemotherapy. Chest 1993; 103: 673-7. [?zet] [PDF]
- Park M, Woo I, Son J, Lee S, Kim D, Mo E, et al. Endobronchial tuberculosis with expectoration of tracheal cartilages. Eur Respir J 2000; 15: 800-2. [?zet] [PDF]
- Rikimaru T. Endobronchial tuberculosis. Expert Rev Anti Infect Ther 2004; 2: 245-51. [?zet]
- Chan H, Sun A, Hoheisel G. Endobronchial tuberculosis-is corticosteroid treatment useful? A report of 8 cases and review of the literature. Postgrad Med J 1990; 66: 822-6. [?zet] [PDF]
- Van den Brande P,? Van de Mierop F, Verbeken E, Demedts M. Clinical spectrum of endobronchial tuberculosis in elderly patients. Arch Intern Med 1990; 150: 2105-8. [?zet]
- Rikimaru T. Therapeutic management of endobronchial tuberculosis. Expert Opin Pharmacother 2004; 5: 1463-70. [?zet]
- Lee J, Chung H. Bronchoscopic, radiologic and pulmonary function evaluation of endobronchial tuberculosis. Respirology 2000; 5: 411-7. [?zet]
- Cakir E, Uyan? ZS, Oktem S, Karakoc F, Ersu R, Karadag B, et al. Flexible bronchoscopy for diagnosis and follow up of childhood endobronchial tuberculosis. Ped Infec Dis J 2008; 27: 783-7. [?zet]
- Al-Maslamani M, Ibrahim WH, Chacko K, Al-Khal A. Endobronchial tuberculosis simulating lung cancer and healing. Libyan J Med 2008, AOP: 080330.
- Araz O, Akg?n M, Sa?lam M, S, ?zden K, Mirici A. The diagnostic value of bronchoscopy in smear negative cases with pulmonary tuberculosis. Tuberk Toraks 2008; 56: 150-7. [?zet] [PDF]
Yaz??ma Adresi (Address for Correspondence):
Dr. Yasemin SAYGIDE?ER
SB D??kap? Y?ld?r?m Beyaz?t E?itim ve Ara?t?rma Hastanesi,
G???s Hastal?klar? Klini?i, Alt?nda?,
ANKARA - TURKEY
e-mail: ysaygideger@gmail.com