A?r?s?z sol hemorajik plevral ef?zyon:
Sakk?ler arkus
aorta anevrizma ka?a??n?n nadir bir prezantasyonu
Mohammed
Azfar SIDDIQUI1, Jamal AKHTAR2, Syed Wajahat Ali RIZVI3,
Syed Amjad Ali RIZVI4, Ibne AHMAD1, Ekramullah1
1 Aligarh Muslim ?niversitesi, Jawaharlal Nehru T?p Fak?ltesi, Radyoloji Anabilim Dal?, Aligarh, Hindistan,
2 Aligarh Muslim ?niversitesi, Jawaharlal Nehru T?p Fak?ltesi, G???s Hastal?klar? ve Tuberk?loz Anabilim Dal?,
Aligarh, Hindistan,
3 Aligarh Muslim ?niversitesi, Jawaharlal Nehru T?p Fak?ltesi, G?z Hastal?klar? Anabilim Dal?, Aligarh, Hindistan,
4 Aligarh Muslim ?niversitesi, Jawaharlal Nehru T?p Fak?ltesi, Cerrahi Anabilim Dal?, Aligarh, Hindistan.
?ZET
A?r?s?z sol hemorajik plevral ef?zyon: Sakk?ler arkus aorta anevrizma ka?a??n?n nadir bir prezantasyonu
Torasik? aort anevrizmalar?n?n ?o?u asemptomatik olup, di?er nedenlerle ?ekilen rutin g???s radyografilerinde tesad?fen saptan?rlar.? Sadece, nadir olarak, s?kl?kla ciddi a?r? ile ba?vuruya neden olan hayat? tehdit eden ka?ak ve diseksiyon varl???nda semptomatik olurlar.? Bu yaz?da, nefes darl???, aral?kl? ?ks?r?k, ate? ve sol tarafl? a?r?s?z hemorajik plevral ef?zyonlu 67 ya??nda bir erkek olguyu sunuyoruz. Radyografi, bilgisayarl? tomografi ve manyetik rezonans g?r?nt?leme ile arkus aorta transvers b?l?m? lateralinden y?kselen bir sakk?ler anevrizma ve sol plevral bo?lukla ili?kili, yalanc? l?menli disseke desendan aort anevrizmas? saptand?. Olgu, cerrahi tedaviyi kabul etmedi ve kan transf?zyonu ve antihipertansif medikasyon ile konservatif olarak tedavi edildi. Sekizinci g?nde, fatal ?ok epizodu nedeniyle kaybedildi. Klinik olarak bron? karsinomunu d???nd?ren, nefes darl???, ?ks?r?k ve ate?le ba?vuran nontravmatik hemorajik plevral ef?zyonlu ya?l? hastalarda ay?r?c? tan?da disekan torasik anevrizman?n yer almas?n? d???n?yoruz. Tan?sal i?lem olarak toraks bilgisayarl? tomografisi acilen ?ekilmelidir.
Anahtar Kelimeler: Aort anevrizmas?, hemoraji, plevral ef?zyon.
SUMMARY
Painless left hemorrhagic pleural effusion: an unusual presentation of leaking saccular aortic arch aneurysm
Mohammed
Azfar SIDDIQUI1, Jamal AKHTAR2, Syed Wajahat Ali RIZVI3,
Syed Amjad Ali RIZVI4, Ibne AHMAD1, Ekramullah1
1 Department of Radiodiagnosis, Jawaharlal Nehru Medical College, Aligarh Muslim University, Aligarh, India,
2 Department of Chest Diseases and Tuberculosis, Jawaharlal Nehru Medical College, Aligarh Muslim University,
Aligarh, India,
3 Department of Ophthalmology, Jawaharlal Nehru Medical College, Aligarh Muslim University, Aligarh, India,
4 Department of Surgery, Jawaharlal Nehru Medical College, Aligarh Muslim University, Aligarh, India.
Most thoracic aortic aneurysms are asymptomatic and are detected by chance on routine chest imaging for some other reasons. Only rarely it is symptomatic due to leak and dissection which is a potentially life threatening event that commonly presents with severe pain. In this report, we present the case of a 67-year-old man who presented with shortness of breath, intermittent cough, fever, and left sided painless hemorrhagic pleural effusion. Further investigation by plain radiography, computed tomography and magnetic resonance imaging revealed a saccular aneurysm arising from the lateral aspect of the mid-transverse arch of the aorta, along with a dissecting descending aortic aneurysm with false lumen communicating with left pleural space. The patient refused any surgical procedure and was treated conservatively with blood transfusions and anti hypertensive medication. On the 8th day patient finally succumb to a fatal episode of shock. We suggest dissecting thoracic aneurysm be included in the differential diagnosis of non-traumatic hemorrhagic pleural effusion in an elderly patient presenting with dysnea, cough and fever, which otherwise suggest the clinical diagnosis of bronchogenic carcinoma. Computed tomography of the chest should be immediately performed as the diagnostic procedure of choice.
Key Words: Aortic aneurysm, hemorrhage, pleural effusion.
Geli? Tarihi/Received: 06/04/2012 - Kabul Edili? Tarihi/Accepted: 16/04/2012
CASE REPORT
A 67-year-old known hypertensive man was admitted to the chest medicine department with complaints of new onset shortness of breath, intermittent cough, and fever without chills. There was no history of sputum, hemoptysis, and chest pain or weight loss. The patient also denied any history of trauma, cyanosis, jaundice or any secondary complication of hypertension. His blood pressure was 156/92 mmHg, and pulse rate was 68 beats/minute. On physical examination there was dullness to percussion and reduced breath sounds at left lung base. There was also decreased movement and diminished vocal fremitus on left side. Cardiac examination did not reveal any abnormalities and his electrocardiogram was also unremarkable.
Biochemical analysis demonstrated normal cardiac enzyme level and presence of normochromic and normocytic anemia with hemoglobin of 10 g/100 mL. Chest X-ray was done, which shows massive left sided effusion and an abnormal convex opacity in the aortopulmonary area with right mediastinal shift (Figure 1A). The patient was put in a propped up bed with moist O2 and IV fluid with cephalosporin and deriphylline was started.
A left thoracocentesis was performed, and it revealed thin, grossly hemorrhagic, reddish pleural fluid that did not clot. Fluid cytology and biochemistry shows plenty of RBCs with elevated neutrophil count. No organisms were identified on Gram's stain or culture, nor were malignant cells identified by cytology.
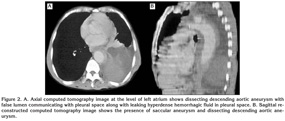
Computed tomography (CT) scan revealed a saccular aneurysm arising from the lateral aspect of the mid-transverse arch of the aorta, along with a dissecting descending aortic aneurysm (Figure 1, 2). An intimal flap was seen separating the true lumina and false lumina, which communicated with the left pleural space. The presence of hyperdense fluid in the left pleural space signified a leaking aortic aneurysm. Magnetic resonance imaging (MRI) was done which confirm the nature of lesion (Figure 3).
Two units of packed RBCs were administered and the patient was treated with propranolol. Cardiothoracic surgery consultation was done which emphasized need for aggressive preoperative management of arterial pressure and prompt surgical intervention. However, patient refused any surgical procedures. On the 8th day of admission, patient condition deteriorated and all resuscitative measures failed with patient dying within four hours of beginning of fatal episode of shock.
DISCUSSION
Aneurysm is a localized or diffuse dilation of an artery with a diameter at least 50% greater then the expected size of the artery (1). In the ascending aorta, a diameter larger than 4 cm while in the descending aorta, a diameter greater than 3 cm is regarded as an aneurysm (2). In a true aneurysm, all of the components of vessel wall are present, whereas a false aneurysm has an incomplete wall. The shape of aneurysm may be fusiform (involve the entire circumference of the aortic wall) or saccular (involve only a portion of the wall).
Aortic dissection is characterized by dissection of blood along the laminar planes of the aortic media, with the formation of a blood-filled channel within the aortic wall. It commonly occurs in two groups of patients (3). The first group consists of older men with long history of hypertension. The second major subgroup consists of younger patients with a systemic or localized abnormality of aortic connective tissue that include aortic coarctation, a bicuspid aortic valve, and disorders of collagen, including Marfan's syndrome, Ehlers-Danlos syndrome, and degeneration of the aortic media.
Most thoracic aortic aneurysms are asymptomatic and are detected by chance on chest X-ray (4). Few cases present with sudden death due to acute rupture. In patients who survive the initial tear, severe pain is a classic presenting symptom. Pain is tearing in nature and located either in the anterior chest, which is suggestive of an ascending aortic dissection, or in the posterior chest or back, which is suggestive of a descending aortic dissection (3). Compressive symptoms like hoarseness of voice, stridor, cough, wheeze, left diaphragmatic palsy, dysphagia, are also reported as presenting symptoms (4). Painless dissection was described only in a minority of the patients, and most of these presented with congestive heart failure, stroke, or syncope (5).
Hemorrhagic pleural effusion may occur in various conditions. The different diagnosis includes traumatic injury, pulmonary infarction, tuberculosis, pulmonary thromboembolism, and pleuropulmonary malignancy. It could also be a presenting sign of acute aortic dissection that is extremely rare (6). Besides our case, only few cases have been reported in literature with such presentation.
Acute aortic dissection is a potentially life-threatening condition requiring immediate assessment. Prompt and accurate diagnosis is required to initiate appropriate surgical repair or medical treatment. Without immediate treatment, the outcome is often fatal with more than 50% of patients dying in the first 48 hours (6). However, misdiagnosis still remains an unresolved problem because of variable and unpredictable clinical presentation.
In the past, angiography was the only accurate examination for evaluating the aorta. Currently, non-invasive radiologic assessment of patients with techniques such as spiral CT, MRI, and transesophageal echocardiography (TEE) is the cornerstone of the diagnostic process (7). A chest X-ray is usually the initial examination performed and reveals pathologic findings such as abnormal aortic contour, widening of mediastinum, displaced intimal calcification, and pleural effusion (8). A contrast-enhanced CT scan currently is the method of choice for the diagnosis and management of patients with suspected dissection because of a diagnostic accuracy comparable with aortography, wide availability, ease of performance, and examination speed (7). Due to continued improvements in technique, MRI and TEE is also being performed in increasing numbers of patients with suspected aortic dissection. Angiographic evaluation is now reserved for only those patients in whom the previously noted studies are equivocal or when additional anatomic information is required especially for those in whom surgery is planned (7). Based on current recommendations most of the uncomplicated descending aortic dissection are treated medically. Surgical approach is reserved for patients with proximal dissection or for cases of distal dissection complicated by rupture, compromise of a major vessel, or recurrent pain (7,9,10).
In summary, our case highlights the unpredictable clinical presentation of a potentially life threating condition, dissecting aortic aneurysm. Although in an elderly male who present with X-ray evidences of massive pleural effusion and hilar mass, bronchogenic carcinoma comes as a most important differential diagnosis, but this case study suggest that aortic dissection, though rare should be kept in mind as a differential diagnosis in these situations.
CONFLICT of INTEREST
None declared.
REFERENCES
- Benjamin ME, Hansen KJ, Craven TE, Keith DR, Plonk GW, Geary RL, et al. Combined aortic and renal artery surgery. A contemporary experience. Ann Surg 1996; 223: 555-65; 565-7. [?zet]
- Erbel R. Diseases of the thoracic aorta. Heart 2001; 86: 227-34. [PDF]
- Little S, Johnson J, Moon BY, Mehta S. Painless left hemorrhagic pleural effusion: an unusual presentation of dissecting ascending aortic aneurysm. Chest 1999; 116: 1478-80. [?zet] [PDF]
- Sengupta P, Mitra B, Saha K, Maitra S, Pal J, Sarkar N. Descending thoracic aortic aneurysm presenting as left sided hemorrhagic pleural effusion. J Assoc Physicians India 2007; 55: 297-300. [?zet]
- Spittell PC, Spittell JA Jr, Joyce JW, Tajik AJ, Edwards WD, Schaff HV, et al. Clinical features and differential diagnosis of aortic dissection: experience with 236 cases (1980 through 1990). Mayo Clin Proc 1993; 68: 642-51. [?zet]
- Chen HY. Rupture of aortic aneurysm with late right hemorrhagic pleural effusion. Am J Emerg Med 2010; 28: 1058.e1-3.
- Gandelman G, Barzilay N, Krupsky M, Resnitzky P. Left pleural hemorrhagic effusion. A presenting sign of thoracic aortic dissecting aneurysm. Chest 1994; 106: 636-8. [?zet] [PDF]
- Slater EE, DeSanctis RW. The clinical recognition of dissecting aortic aneurysm. Am J Med 1976; 60: 625-33. [?zet]
- Glower DD, Speier RH, White WD, Smith LR, Rankin JS, Wolfe WG. Management and long-term outcome of aortic dissection. Ann Surg 1991; 214: 31-41. [?zet] [PDF]
- Glower DD, Fann JI, Speier RH, Morrison L, White WD, Smith LR, et al. Comparison of medical and surgical therapy for uncomplicated descending aortic dissection. Circulation 1990; 82(Suppl 5): IV39-46. [?zet]
Yaz??ma Adresi (Address for Correspondence):
Dr. Mohammed Azfar Siddiqui,
Department of Radiodiagnosis,
Jawaharlal Nehru Medical College,
Aligarh Muslim University,
Aligarh - INDIA
e-mail: drazfarsiddiqui@gmail.com