Bir ?ocuk hastada akci?er apsesi olarak prezente olan konjenital kistik adenomatoid malformasyon
K. Jagadish Kumar1, Anilkumar MG2, Shivamurthy YL1, Prashanth Kumar M2
1 JSS T?p Koleji, Pediatri B?l?m?, Mysore, Hindistan,
2 JSS T?p Koleji, Pediatrik Cerrahi B?l?m?, Mysore, Hindistan.
?ZET
Bir ?ocuk hastada akci?er apsesi olarak prezente olan konjenital kistik adenomatoid malformasyon
Konjenital kistik adenomatoid malformasyon, farkl? boyut veya da??l?ml? anormal bron?iyoler yap? varl??? ile karakterize hamartamat?z kistik akci?er lezyonlar?d?r. Olgular?n ?o?unda, solunum s?k?nt?s? neonatal d?nemde g?r?l?r ve hastalar?n yakla??k %90'?nda tan?, solunum yolu infeksiyonlar?na ba?l? olarak iki ya??ndan ?nce? konulur. Biz, akci?er apsesi ?eklinde prezente olan, klinik olarak ampiyemi taklit eden ?? ya? alt? ayl?k konjenital kistik adenomatoid malformasyonlu bir erkek hastay? sunuyoruz. Olguya lobektomi yap?ld? ve takipte sorunsuz izleniyor.
Anahtar Kelimeler: KKAM, akci?er apsesi, ?? ya? alt? ay, lobektomi.
SUMMARY
Congenital cystic adenomatoid malformation presenting as lung abscess in a child
K. Jagadish Kumar1, Anilkumar MG2, Shivamurthy YL1, Prashanth Kumar M2
1 Department of Pediatrics, JSS Medical College, Mysore, India,
2 Department of Pediatrics Surgery, JSS Medical College, Mysore, India.
Congenital cystic adenomatoid malformation composes of hamartomatous cystic lung lesions characterised by the presence of abnormal bronchiolar structures of varying sizes or distribution. In most of the cases, respiratory distress occurs during the neonatal period, and in about 90% of patients, congenital cystic adenomatoid malformation is diagnosed before the age of two years due to respiratory infection. We describe a case of congenital cystic adenomatoid malformation presenting as lung abscess in a 3-year six months old male clinically mimicking empyema. He undergone lobectomy and doing well in the follow-up.
Key Words: CCAM, lung abscess, three years six months, lobectony.
Geli? Tarihi/Received: 07/09/2012 - Kabul Edili? Tarihi/Accepted: 20/09/2012
Introduction
Congenital cystic adenomatoid malformation (CCAM) of the lung is an uncommon fetal development anomaly of the terminal respiratory structures. The reported incidence of CCAM is 1 in 25.000-35.000 pregnancies (1). CCAM is the second most common congenital lung lesion in children (2,3). Prenatal diagnosis is possible by ultrasonography after the 16 week of gestation (1). CCAM most commonly present as respiratory distress in the neonatal period and up to 90% of diagnosis are made within the first two years of life (2,4). It may remain asymptomatic or in late childhood or in adult life, it can present as recurrent chest infections or even undergo malignant transformation (1,2,5). It comprises of heterogeneous group of cystic and non-cystic lung lesions classified into three types by Stocker et al. and Type I (macrocystic type) accounts for 50% to 70% of cases (6). We report a case of CCAM presenting as lung abscess of the right lower lobe in a 3-year six months old male clinically mimicking empyema. The case is unusual due to normal prenatal ultrasonography, the late age of onset without prior recurrent chest infections and lung abscess in CCAM.
Case Report
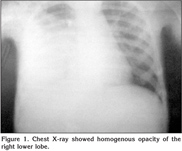
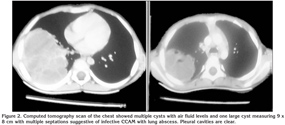
A 3-years six month old boy presented with fever since 15 days and cough since three days. There was no history of recurrent chest infections, hemoptysis, chest trauma, foreign body aspiration or chronic cough. On examination, he was febrile 103?F, RR 40/min, PR 106/min and BP 90/60 mmHg. He was sick, there was no cyanosis, clubbing or lymphadenopathy. His oxygen saturation was 92% in room air. His weight was 11 kg (< 5th percentile) and his height was 86 cm (< 5th percentile). Respiratory system examination revealed decreased movements on right side, diminished tactile fremitus with dullness on percussion at right infra scapular and axillary areas. Auscultation of the chest revealed decreased breath sound and decreased vocal resonance in the right infra scapular and axillary areas. Other systems examination was unremarkable. Clinically diagnosis of right pleural effusion/empyema was made. Investigations: -Hb 11.1 g/dL, Hct 34%, TLC 31.700/mm3, Neutrophils 74%, Lymphocytes 26%, platelets 700.000/mm3, ESR 60 mm, CRP 178 and blood culture was sterile. Chest X-ray showed homogenous opacity of the right lower lobe (Figure 1). Computed tomography (CT) scan of the chest showed multiple cysts with air fluid levels and one large cyst measuring 9 x 8 cm with multiple septations suggestive of infective CCAM with lung abscess. Pleural cavities are clear (Figure 2). She was started on inj ceftraiaxone and inj linezolid. The child underwent right thoracotomy and 70 mL thick pus was drained from the lung abscess and right lower lobectomy was done. Pus culture was sterile and negative for acid fast bacillus. He became afebrile after three days of lobectomy. He was given 14 days of antibiotics and discharged. Macroscopic examination revealed a lung lobe measuring 9.5 x 7.5 x 2 cm and cut section showed a large cystic cavity measuring 7.5 x 4 x 2 cm with a shaggy inner surface with surrounding yellow grayish areas. Microscopy of the lung showed many interconnected cysts lined by pseudostratified columnar epithelium with mucous secreting glands with abundant inflammatory cells suggestive of type-1 CCAM.
Discussion
CCAM is usually diagnosed antenatally by imaging techniques, representing about 25% of all congenital lung lesions (4,7). CCAM is the most common type of fetal thoracic mass diagnosed by prenatal ultrasonography and can be diagnosed after the 16th week of gestation (1,7). CCAM are most commonly diagnosed in the neonatal period and up to 90% of diagnoses are made in the first two years of life (1,2,4). There are three types of clinical presentations in most CCAMs of considerable size.
a. During pregnancy as hydrops, preeclampsia or polyhydramnios.
b. In the neonatal period as respiratory distress. This is the most common mode of presentation and the respiratory distress is secondary to the cyst expanding and compressing its surrounding structures
c. Silent both during pregnancy and at birth, and in whom clinical onset was later than at the age of six months (7). In the latter type late complications, such as recurrent pneumonia, abscess formation, spontaneous pneumothorax, haemoptysis, or coincidental discovery on a chest radiograph may lead to the diagnosis (2). In a study by Lujan et al; out of 12 late onset CCAM cases 75% presented with repeated lung infections,16% a chance finding and 8% had pneumothorax (7). However our child did not have recurrent chest infections, presented with symptoms for the first time after two years of age, clinically and chest X-ray wise diagnosed as pneumonia/empyema but CT wise lung abscess. Infact ultrasonography was done during pregnancy in our child, but CCAM was missed. Although ultrasonographic prenatal diagnosis is becoming increasingly sophisticated, diagnostic errors are possible and some patients suffering from CCAM of reduced size are not diagnosed (7). These patients remain asymptomatic until the occurrence of respiratory infections. Repeated infections can be explained by impossibility of draining the secretions formed in the cysts and the colonization by the microorganisms (7). Our case was diagnosed radiologically as pneumonia/empyema. The infectious presentation of our CCAM child was radiologically indistinguishable from a conventional pneumonia/empyema. Those CCAM cases who present as pneumonias, the chest X-ray was indistinguishable from that of pneumonia unless it shows an air-fluid level (7). In fact, some small CCAMs appear normal on the chest X-ray and are only detectable by chest CT (7). If CCAM is not suspected, the diagnosis may be missed until reinfection. Diagnosis becomes easy when the residual radiological images persist even after clinical improvement (7). Differential diagnosis of CCAM include other cystic lesions like pulmonary sequestration, bronchogenic cyst, congenital lobar emphysema, diaphragmatic hernia and cystic bronchiectasis (1). When the cystic lesion is single in CCAM, the differential diagnosis with the congenital parenchymal and bronchogenic cysts is not possible by CT scan alone because of similar imaging features (2). The diagnostic method of choice is the CT scan but the definitive diagnosis of CCAM is made only on histologic examination (1,7). CT is useful in confirming the presence and determining the extent of the lesion. Bronchogenic cysts are generally extrapulmonary, usually located in the right paratracheal or carenal region whereas CCAM is always intrapulmonary. The histology of bronchogenic and lung cysts shows a columnar to cuboidal respiratory epithelial lining, surrounded by a fibromuscular wall which contains islands of cartilage and nests of bronchial glands (2). The wall of single cyst of CCAM type I is free of cartilage (6). Lujan et al. advocate surgical resection as the treatment, in principle a lobectomy or a segmentectomy, in highly selected cases. Localized resections should be avoided because of the risk of recurrence (7). In view of asymptomatic lesions have the potential to become infected, can undergo malignant transformation, or cause pneumothorax surgical resection is the treatment of choice (5,8,9,10).
In conclusion, late onset CCAM is an infrequent illness which requires a strong index of suspicion to make a diagnosis. Eventhough CCAM usually presents with recurrent pulmonary infections, lung abscess presentation is not uncommon. Early recognition and surgical treatment of CCAM is essential to prevent the consequences of recurrent pulmonary infections and the potential risk for malignant transformation.
CONFLICT of INTEREST
None declared.
REFERENCES
- Sirithangkul S, Chuengchitraks S, Staworn D, Laohapand C, Silarat T. Late manifestation of congenital cystic adenomatoid malformation with lung abscess: a case report. J Med Assoc Thai 2010; 93(Suppl 6): 223-7.
- Morelli L, Piscioli I, Licci S, Donato S, Catalucci A, Del Nonno F. Pulmonary congenital cystic adenomatoid malformation, type I, presenting as a single cyst of the middle lobe in an adult: case report. Diagn Pathol 2007; 2: 17.
- Mohta A, Kanojia RP, Bathla S, Khurana N. Cystic adenomatoid malformation of the lung: a diagnostic dilemma. Afr J Paediatr Surg 2009; 6: 112-3.
- Ayadi-Kaddour A, Chaabouni S, Mera? S, Ben Mrad S, Djilani H, Tritar F, et al. Congenital cystic adenomatoid malformation of the lung. Report of 3 cases with late presentation. Rev Mal Respir 2008; 25: 338-43.
- Granata C, Gambini C, Balducci T, Toma P, Michelazzi A, Conte M, et al. Bronchioalveolar carcinoma arising in congenital cystic adenomatoid malformation in a child: a case report and review of malignancies originating in congenital cystic adenomatoid malformation. Pediatr Pulmonol 1998; 25: 62-6.
- Stocker JT. Congenital pulmonary airway malformation: a new name for and an expanded classification of congenital cystic adenomatous malformation of the lung. Histopathology 2002; 41(Suppl 2): 424-31.
- Lujan M, Bosque M, Mirapeix RM, Marco MT, Asensio O, Domingo C. Late-Onset congenital cystic adenomatoid malformation of the lung. Embryology, clinical symptomatology, diagnostic procedures, therapeutic approach and clinical follow-up. Respiration 2002; 69: 148-54.
- Collins AM, Ridgway PF, Killeen RP, Dodd JD, Tolan M. Congenital cystic adenomatoid malformation of the lung: hazards of delayed diagnosis. Respirology 2009; 14: 1058-60.
- Wong A, Vieten D, Singh S, Harvey JG, Holland AJ. Long-term outcome of asymptomatic patients with congenital cystic adenomatoid malformation. Pediatr Surg Int 2009; 25: 479-85.
- Mathai AM, Kini H, Pai MR, Shetty AB, Murali N. Congenital cystic adenomatoid malformation of lung type 1. J Pediatr Surg 2010; 45: 25-8.
Yaz??ma Adresi (Address for Correspondence):
Dr. K. Jagadish Kumar,
Department of Pediatrics,
JSS Medical College,
MYSORE - INDIA
e-mail: jagdishmandya@gmail.com